Correlations of interleukin-17 and regulatory T cells with the severity of chronic obstructive pulmonary disease and pulmonary function.
Correlación de la interleucina-17 y las células T reguladoras con la gravedad de la enfermedad pulmonar obstructiva crónica y la función pulmonar.
Resumen
Nuestro objetivo fue explorar las correlaciones entre la interleucina-17 (IL-17) y las células T reguladoras (Treg), así como entre la gravedad de la enfermedad pulmonar obstructiva crónica (EPOC) y la función pulmonar. Se compararon los datos de un grupo con EPOC (pacientes con EPOC tratados entre junio de 2020 y septiembre de 2023, n=90), un grupo de fumadores (fumadores sanos, n=90) y un grupo control (no fumadores sanos, n=90). El grupo de EPOC presentó el nivel más alto de IL-17 y el recuento más bajo de células Treg CD4+, CD25+ y CD4+CD25+ en la sangre periférica, seguido por los grupos de fumadores y de control (p<0,05). El recuento de células Treg CD4+, células Treg CD25+, células Treg CD4+CD25+, la capacidad vital forzada (FVC), el volumen espiratorio forzado en el primer segundo (FEV1) y la relación FEV1/FVC fueron más altos en el grupo leve de EPOC, seguido por los grupos moderado y severo (p<0,05). El recuento de células Treg CD4+, células Treg CD25+ y células Treg CD4+CD25+ mostró correlaciones positivas con FEV1, FVC y FEV1 /FVC (r>0, p<0,05) y correlaciones negativas con el nivel de IL-17 (r<0, p<0,05). El nivel de IL-17 se correlacionó negativamente con FEV1, FVC y FEV1 /FVC (r<0, p<0,05). La detección combinada de IL-17 y de subconjuntos de Treg es útil para aumentar el valor predictivo de estos en la aparición de EPOC.
Descargas
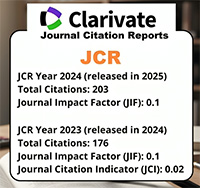
Citas
Terry PD, Dhand R. Inhalation Therapy for Stable COPD: 20 Years of GOLD Reports. Adv Ther. 2020; 37(5): 1812-1828. https://doi.org/10.1007/s12325-020-01289-y
Yang IA, Jenkins CR, Salvi SS. Chronic obstructive pulmonary disease in never-smokers: risk factors, pathogenesis, and implications for prevention and treatment. Lancet Respir Med. 2022; 10(5): 497-511. https://doi.org/10.1016/S2213-2600(21)00506-3
Qin K, Xu B, Pang M, Wang H, Yu B. The functions of CD4 T-helper lymphocytes in chronic obstructive pulmonary disease. Acta Biochim Biophys Sin. 2022; 54(2): 173-178. https://doi.org/10.3724/abbs.2021009
Ma R, Su H, Jiao K, Liu J. Role of Th17 cells, Treg cells, and Th17/Treg imbalance in immune homeostasis disorders in patients with chronic obstructive pulmonary disease. Immun Inflamm Dis. 2023; 11(2): e784. https://doi.org/10.1002/iid3.784
Thomas R, Qiao S, Yang X. Th17/Treg Imbalance: Implications in Lung Inflammatory Diseases. Int J Mol Sci. 2023; 24(5): 4865. https://doi.org/10.3390/ijms24054865
Ritzmann F, Lunding LP, Bals R, Wegmann M, Beisswenger C. IL-17 Cytokines and Chronic Lung Diseases. Cells. 2022; 11(14): 2132. https://doi.org/10.3390/cells11142132
Singh D, Agusti A, Anzueto A, Barnes PJ, Bourbeau J, Celli BR, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease: the GOLD science committee report 2019. Eur Respir J. 2019;53(5):1900164. https://doi.org/10.1183/13993003.00164-2019
Christenson SA, Smith BM, Bafadhel M, Putcha N. Chronic obstructive pulmonary disease. Lancet. 2022; 399(10342): 2227-2242. https://doi.org/10.1016/S0140-6736(22)00470-6
Zhang X, Li X, Ma W, Liu F, Huang P, Wei L, et al. Astragaloside IV restores Th17/Treg balance via inhibiting CXCR4 to improve chronic obstructive pulmonary disease. Immunopharmacol Immunotoxicol. 2023; 45(6): 682-691. https://doi.org/10.1080/08923973.202 3.2228479
Cervilha DAB, Ito JT, Lourenço JD, Olivo CR, Saraiva-Romanholo BM, Volpini RA, et al. The Th17/Treg Cytokine Imbalance in Chronic Obstructive Pulmonary Disease Exacerbation in an Animal Model of Cigarette Smoke Exposure and Lipopolysaccharide Challenge Association. Sci Rep. 2019; 9(1): 1921. https://doi.org/10.1038/s41598-019-38600-z
Henen C, Johnson EA, Wiesel S. Unleashing the Power of IL -17: A Promising Frontier in Chronic Obstructive Pulmonary Disease (COPD) Treatment. Cureus. 2023; 15(7): e41977. https://doi.org/10.7759/cureus.41977
Kubysheva N, Boldina M, Eliseeva T, Soodaeva S, Klimanov I, Khaletskaya A, et al. Relationship of Serum Levels of IL-17, IL-18, TNF-α, and Lung Function Parameters in Patients with COPD, Asthma-COPD Overlap, and Bronchial Asthma. Mediators Inflamm. 2020; 2020: 4652898. https://doi.org/10.1155/2020/4652898
Ding F, Han L, Fu Q, Fan X, Tang R, Lv C, et al. IL-17 Aggravates Pseudomonas aeruginosa Airway Infection in Acute Exacerbations of Chronic Obstructive Pulmonary Disease. Front Immunol. 2022; 12:811803. https://doi.org/10.3389/fimmu.2021.811803
Zhang XF, Xiang SY, Lu J, Li Y, Zhao SJ, Jiang CW, et al. Electroacupuncture inhibits IL -17/IL -17R and post-receptor MAPK signaling pathways in a rat model of chronic obstructive pulmonary disease. Acupunct Med. 2021; 39(6): 663-672. https://doi.org/10.11 77/0964528421996720
Upadhyay P, Wu CW, Pham A, Zeki AA, Royer CM, Kodavanti UP, et al. Animal models and mechanisms of tobacco smoke-induced chronic obstructive pulmonary disease (COPD). J Toxicol Environ Health B Crit Rev. 2023; 26(5): 275-305. https://doi.org/10.1080/10937404.2023.2208886
Jia Y, He T, Wu D, Tong J, Zhu J, Li Z, Dong J. The treatment of Qibai Pingfei Capsule on chronic obstructive pulmonary disease may be mediated by Th17/Treg balance and gut-lung axis microbiota. J Transl Med. 2022; 20(1): 281. https://doi.org/10.1186/s12967-022-03481-w
Zhang D, Liu H, Zhao F, Guo P, Li J, Lu T, et al. Exploring the relationship between Treg-mediated risk in COPD and lung cancer through Mendelian randomization analysis and scRNA-seq data integration. BMC Cancer. 2024; 24(1): 453. https://doi.org/10.1186/s12885-024-12076-1
Silva LEF, Lourenço JD, Silva KR, Santana FPR, Kohler JB, Moreira AR, et al. Th17/Treg imbalance in COPD development: suppressors of cytokine signaling and signal transducers and activators of transcription proteins. Sci Rep. 2020; 10(1): 15287. https://doi.org/10.1038/s41598-020-72305-y
Ito JT, Cervilha DAB, Lourenço JD, Gonçalves NG, Volpini RA, Caldini EG, et al. Th17/Treg imbalance in COPD progression: A temporal analysis using a CS-induced model. PLoS One. 2019; 14(1): e0209351. https://doi.org/10.1371/journal.pone.0209351
Liao SX, Chen J, Zhang LY, Zhang J, Sun PP, Ou-Yang Y. Effects of SOCS1-overex- pressing dendritic cells on Th17- and Tregrelated cytokines in COPD mice. BMC Pulm Med. 2022; 22(1): 145. https://doi.org/10.1186/s12890-022-01931-1