Comprehensive analysis of autophagy- and glycolysis-related differentially expressed genes involved in chronic inflammation in obese patients.
Análisis exhaustivo de los genes expresados diferencialmente, relacionados con la autofagia y la glucólisis, que intervienen en la inflamación crónica en pacientes obesos.
Resumen
La interacción entre la glucólisis y la autofagia contribuye a la reprogramación de la inflamación crónica en la obesidad, pero el conocimiento sobre esta interacción es limitado. Se utilizaron datos públicamente disponibles para analizar los genes expresados diferencialmente relacionados con la autofagia y la glucólisis (A&GRDEG) entre pacientes con obesidad y con peso normal en dos conjuntos de datos. Se obtuvo un total de 5 A&GRDEG mediante cribado, a saber: la proteína recombinante de unión al factor de iniciación de la traducción eucariótica 4E 1 (EIF4EBP1), el factor de crecimiento transformante beta 1 (TGFB1), la sintasa de ácidos grasos (FASN), la alfa-sinucleína (SNCA) y el receptor de quimiocina C-X-C 4 (CXCR4). Los niveles de autofagia y de glucólisis mostraron un valor predictivo elevado para el desarrollo de la obesidad y contribuyen mecánicamente a la patogénesis de la enfermedad mediante la desregulación inmunometabólica.
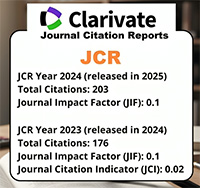
Descargas
Citas
Kim DS, Scherer PE. Obesity, Diabetes, and Increased Cancer Progression. Diabetes Metab J. 2021;45(6):799-812. https://doi.org/10.4093/dmj.2021.0077.
Calle EE, Kaaks R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer. 2004;4(8):579-591. https://doi.org/10.1038/nrc1408.
Namkoong S, Cho CS, Semple I, Lee JH. Autophagy Dysregulation and Obesity-Associated Pathologies. Mol Cells. 2018;41(1):3-10. https://doi.org/10.14348/molcells.2018.2213.
Tooze SA, Dikic I. Autophagy Captures the Nobel Prize. Cell. 2016;167(6):1433-1435. https://doi.org/10.1016/j.cell.2016.11.023.
Zhang Y, Sowers JR, Ren J. Targeting autophagy in obesity: from pathophysiology to management. Nat Rev Endocrinol. 2018;14(6):356-376. https://doi.org/10.1038/s41574-018-0009-1.
Dann SG, Selvaraj A, Thomas G. mTOR Complex1-S6K1 signaling: at the crossroads of obesity, diabetes and cancer. Trends Mol Med. 2007;13(6):252-259. https://doi.org/10.1016/j.molmed.2007.04.002.
Behrooz AB, Cordani M, Fiore A, Donadelli M, Gordon JW, Klionsky DJ, et al. The obesity-autophagy-cancer axis: Mechanistic insights and therapeutic perspectives. Semin Cancer Biol. 2024;99:24-44. https://doi.org/10.1016/j.semcancer.2024.01.003.
Soto-Heredero G, Gomez de Las Heras MM, Gabande-Rodriguez E, Oller J, Mittelbrunn M. Glycolysis a key player in the inflammatory response. FEBS J. 2020;287(16):3350-3369. https://doi.org/10.1111/febs.15327.
Chang CH, Curtis JD, Maggi LB, Jr., Faubert B, Villarino AV, O’Sullivan D, et al. Posttranscriptional control of T cell effector function by aerobic glycolysis. Cell. 2013;153(6):1239-1251. https://doi.org/10.1016/j.cell.2013.05.016.
Jiao P, Chen Q, Shah S, Du J, Tao B, Tzameli I, et al. Obesity-related upregulation of monocyte chemotactic factors in adipocytes: involvement of nuclear factor- kappaB and c-Jun NH2-terminal kinase pathways. Diabetes. 2009;58(1):104-115. https://doi.org/10.2337/db07-1344.
O’Rourke RW, White AE, Metcalf MD, Olivas AS, Mitra P, Larison WG, et al. Hypoxiainduced inflammatory cytokine secretion in human adipose tissue stromovascular cells. Diabetologia. 2011;54(6):1480-1490. https://doi.org/10.1007/s00125-011-2103-y.
Boutens L, Hooiveld GJ, Dhingra S, Cramer RA, Netea MG, Stienstra R. Unique metabolic activation of adipose tissue macrophages in obesity promotes inflammatory responses. Diabetologia. 2018;61(4):942-953. https://doi.org/10.1007/s00125-017-4526-6.
Jacks RD, Lumeng CN. Macrophage and T cell networks in adipose tissue. Nat Rev Endocrinol. 2024;20(1):50-61. https://doi.org/10.1038/s41574-023-00908-2.
Gancheva S, Ouni M, Jelenik T, Koliaki C, Szendroedi J, Toledo FGS, et al. Dynamic changes of muscle insulin sensitivity after metabolic surgery. Nat Commun. 2019;10(1):4179. https://doi.org/10.1038/s41467-019-12081-0.
Petrus P, Mejhert N, Corrales P, Lecoutre S, Li Q, Maldonado E, et al. Transforming Growth Factor-β3 Regulates Adipocyte Number in Subcutaneous White Adipose Tissue. Cell Rep. 2018;25(3):551-560.e5. https://doi.org/10.1016/j.celrep.2018.09.069.
Sun S, Shen Y, Wang J, Li J, Cao J, Zhang J. Identification and Validation of Autophagy-Related Genes in Chronic Obstructive Pulmonary Disease. Int J Chron Obstruct Pulmon Dis. 2021;16:67-78. https://doi.org/10.2147/copd.S288428.
Fu D, Zhang B, Wu S, Zhang Y, Xie J, Ning W, et al. Prognosis and Characterization of Immune Microenvironment in Acute Myeloid Leukemia Through Identification of an Autophagy-Related Signature. Front Immunol. 2021;12:695865. https://doi.org/10.3389/fimmu.2021.695865.
Wang N, Wei L, Liu D, Zhang Q, Xia X, Ding L, et al. Identification and Validation of Autophagy-Related Genes in Diabetic Retinopathy. Front Endocrinol (Lausanne). 2022;13:867600. https://doi.org/10.3389/fendo.2022.867600.
Zhang D, Zheng Y, Yang S, Li Y, Wang M, Yao J, et al. Identification of a Novel Glycolysis-Related Gene Signature for Predicting Breast Cancer Survival. Front Oncol. 2020;10:596087. https://doi.org/10.3389/fonc.2020.596087.
Zheng J, Guo J, Zhu L, Zhou Y, Tong J. Comprehensive analyses of glycolysis-related lncRNAs for ovarian cancer patients. J Ovarian Res. 2021;14(1):124. https://doi.org/10.1186/s13048-021-00881-2.
Bi J, Bi F, Pan X, Yang Q. Establishment of a novel glycolysis-related prognostic gene signature for ovarian cancer and its relationships with immune infiltration of the tumor microenvironment. J Transl Med. 2021;19(1):382. https://doi.org/10.1186/s12967-021-03057-0.
Saltiel AR, Olefsky JM. Inflammatory mechanisms linking obesity and metabolic disease. J Clin Invest. 2017;127(1):1-4. https://doi.org/10.1172/JCI92035.
Zhang T, Linghu KG, Tan J, Wang M, Chen D, Shen Y, et al. TIGAR exacerbates obesity by triggering LRRK2-mediated defects in macroautophagy and chaperone-mediated autophagy in adipocytes. Autophagy. 2024;20(8):1741-1761. https://doi.org/10.1080/15548627.2024.2338576.
Bjornsti MA, Houghton PJ. Lost in translation: dysregulation of cap-dependent translation and cancer. Cancer Cell. 2004;5(6):519-523. https://doi.org/10.1016/j.ccr.2004.05.027.
Chen C, Chen W, Nong Z, Nie Y, Chen X, Pan X, et al. Hyperbaric oxygen alleviated cognitive impairments in mice induced by repeated cerebral ischemia-reperfusion injury via inhibition of autophagy. Life Sci. 2020;241:117170. https://doi.org/10.1016/j.lfs.2019.117170.
Selvarajah B, Azuelos I, Plate M, Guillotin D, Forty EJ, Contento G, et al. mTORC1 amplifies the ATF4-dependent de novo serine-glycine pathway to supply glycine during TGF-beta(1)-induced collagen biosynthesis. Sci Signal. 2019;12(582):eaav3048. https://doi.org/10.1126/scisignal.aav3048.
Le Bacquer O, Petroulakis E, Paglialunga S, Poulin F, Richard D, Cianflone K, et al. Elevated sensitivity to diet-induced obesity and insulin resistance in mice lacking 4E-BP1 and 4E-BP2. J Clin Invest. 2007;117(2):387-396. https://doi.org/10.1172/JCI29528.
Tsai S, Sitzmann JM, Dastidar SG, Rodriguez AA, Vu SL, McDonald CE, et al. Muscle-specific 4E-BP1 signaling activation improves metabolic parameters during aging and obesity. J Clin Invest. 2015;125(8):2952-2964. https://doi.org/10.1172/JCI77361.
Hu X, Jia X, Xu C, Wei Y, Wang Z, Liu G, et al. Downregulation of NK cell activities in Apolipoprotein C-III-induced hyperlipidemia resulting from lipid-induced metabolic reprogramming and crosstalk with lipid-laden dendritic cells. Metabolism. 2021;120:154800. https://doi.org/10.1016/j.metabol.2021.154800.
Siapoush S, Rezaei R, Alavifard H, Hatami B, Zali MR, Vosough M, et al. Therapeutic implications of targeting autophagy and TGF-beta crosstalk for the treatment of liver fibrosis. Life Sci. 2023;329:121894. https://doi.org/10.1016/j.lfs.2023.121894.
Ahamed J, Laurence J. Role of Platelet-Derived Transforming Growth Factor-beta1 and Reactive Oxygen Species in Radiation-Induced Organ Fibrosis. Antioxid Redox Signal. 2017;27(13):977-988. https://doi.org/10.1089/ars.2017.7064.
Hewitson TD, Smith ER. A Metabolic Reprogramming of Glycolysis and Glutamine Metabolism Is a Requisite for Renal Fibrogenesis-Why and How? Front Physiol. 2021;12:645857. https://doi.org/10.3389/fphys.2021.645857.
Yadav H, Quijano C, Kamaraju AK, Gavrilova O, Malek R, Chen W, et al. Protection from obesity and diabetes by blockade of TGF-beta/Smad3 signaling. Cell Metab. 2011;14(1):67-79. https://doi.org/10.1016/j.cmet.2011.04.013.
Bruno A, Di Sano C, Simon HU, Chanez P, Patti AM, Di Vincenzo S, et al. Leptin and TGF-beta1 Downregulate PREP1 Expression in Human Adipose-Derived Mesenchymal Stem Cells and Mature Adipocytes. Front Cell Dev Biol. 2021;9:700481. https://doi.org/10.3389/fcell.2021.700481.
Matsukawa T, Yagi T, Uchida T, Sakai M, Mitsushima M, Naganuma T, et al. Hepatic FASN deficiency differentially affects nonalcoholic fatty liver disease and diabetes in mouse obesity models. JCI In-sight. 2023;8(17):e161282. https://doi.org/10.1172/jci.insight.161282.
Albiges L, Hakimi AA, Xie W, McKay RR, Simantov R, Lin X, et al. Body Mass Index and Metastatic Renal Cell Carcinoma: Clinical and Biological Correlations. J Clin Oncol. 2016;34(30):3655-3663. https://doi.org/10.1200/JCO.2016.66.7311.
Khandekar MJ, Cohen P, Spiegelman BM. Molecular mechanisms of cancer development in obesity. Nat Rev Cancer. 2011;11(12):886-895. https://doi.org/10.1038/nrc3174.
Ross OA, Braithwaite AT, Skipper LM, Kachergus J, Hulihan MM, Middleton FA, et al. Genomic investigation of alpha-synuclein multiplication and parkinsonism. Ann Neurol. 2008;63(6):743-750. https://doi.org/10.1002/ana.21380.
Malpartida AB, Williamson M, Narendra DP, Wade-Martins R, Ryan BJ. Mitochondrial Dysfunction and Mitophagy in Parkinson’s Disease: From Mechanism to Therapy. Trends Biochem Sci. 2021;46(4):329-343. https://doi.org/10.1016/j.tibs.2020.11.007.
Rotermund C, Truckenmuller FM, Schell H, Kahle PJ. Diet-induced obesity accelerates the onset of terminal phenotypes in alpha-synuclein transgenic mice. J Neurochem. 2014;131(6):848-858. https://doi.org/10.1111/jnc.12813.
Chen J, Bai Y, Xue K, Li Z, Zhu Z, Li Q, et al. CREB1-driven CXCR4(hi) neutrophils promote skin inflammation in mouse models and human patients. Nat Commun. 2023;14(1):5894. https://doi.org/10.1038/s41467-023-41484-3.
Yang S, Wei J, Cui YH, Park G, Shah P, Deng Y, et al. m(6)A mRNA demethylase FTO regulates melanoma tumorigenicity and response to anti-PD-1 blockade. Nat Commun. 2019;10(1):2782. https://doi.org/10.1038/s41467-019-10669-0.
Liao YX, Lv JY, Zhou ZF, Xu TY, Yang D, Gao QM, et al. CXCR4 blockade sensitizes osteosarcoma to doxorubicin by inducing autophagic cell death via PI3K‑Akt‑mTOR pathway inhibition. Int J Oncol. 2021;59(1):49. https://doi.org/10.3892/ijo.2021.5229.
Esser N, Legrand-Poels S, Piette J, Scheen AJ, Paquot N. Inflammation as a link between obesity, metabolic syndro- me and type 2 diabetes. Diabetes Res Clin Pract. 2014;105(2):141-150. https://doi.org/10.1016/j.diabres.2014.04.006.
Foretz M, Guigas B, Viollet B. Understan- ding the glucoregulatory mechanisms of met- formin in type 2 diabetes mellitus. Nat Rev Endocrinol. 2019;15(10):569-589. https://doi.org/10.1038/s41574-019-0242-2.
Huus KE, Petersen C, Finlay BB. Diversity and dynamism of IgA-microbiota interac- tions. Nat Rev Immunol. 2021;21(8):514- 525. https://doi.org/10.1038/s41577-021-00506-1.
Ferrucci L, Fabbri E. Inflammageing: chronic inflammation in ageing, cardio- vascular disease, and frailty. Nat Rev Cardiol. 2018;15(9):505-522. https://doi.org/10.1038/s41569-018-0064-2.