The role of amyloid and tau biomarkers in assessing the effectiveness of drug treatment for Alzheimer’s disease.
El papel de los biomarcadores de amiloide y tau en la evaluación de la eficacia del tratamiento farmacológico para la enfermedad de Alzheimer.
Resumen
El objetivo de este estudio es explorar el papel de los biomar- cadores de amiloide y tau en la evaluación de la eficacia de la farmacoterapia para la enfermedad de Alzheimer (EA). Se realizó un análisis retrospectivo de 150 pacientes con EA ingresados en nuestro hospital entre octubre de 2022 y enero de 2024, y se seleccionaron 50 personas sanas como grupo control. Se compararon la información básica, la función cognitiva, la capacidad para realizar las actividades de la vida diaria, así como los biomarcadores de ami- loide y tau entre ambos grupos. Los pacientes con EA fueron tratados con tabletas de hidrocloruro de donepezilo y memantina, y se dividieron en un grupo de pacientes que respondieron al tratamiento y otro grupo de pacien- tes que no respondieron, en función de la eficacia del mismo. Se utilizó un análisis de regresión logística binaria para identificar los factores que afectan la eficacia del tratamiento farmacológico de la EA, y se evaluó la precisión predictiva mediante curvas ROC. Los resultados de este estudio revelan que, en comparación con el grupo control, en el grupo de EA, las puntuaciones en las escalas MMSE, MoCA y los niveles de Aβ1-42 disminuyeron, mientras que los niveles de T-tau y P-Tau-181 aumentaron (p<0,05). Después del tratamien- to farmacológico, 107 de los 150 pacientes con EA mostraron una respuesta favorable. Los años de educación, el ejercicio diario, los niveles de Aβ1-42, T-tau y P-Tau-181 son todos factores que afectan la eficacia del tratamiento farmacológico de la EA. Los cambios en los niveles séricos de Aβ1-42, T-tau y P-Tau-181 pueden servir para evaluar la eficacia del tratamiento farmacológi- co de la EA, con valores de área bajo la curva (AUC) de 0,869, 0,815 y 0,800, respectivamente. La evaluación combinada de estos tres factores tiene un AUC de 0,977. La farmacoterapia puede mejorar la eficacia clínica en la mayo- ría de los pacientes con EA. Los años de educación, el ejercicio, los niveles de Aβ1-42, T-tau y P-Tau-181 son los factores que influyen en la eficacia del trata- miento farmacológico de la EA. La eficacia del tratamiento farmacológico de la EA puede evaluarse detectando los cambios en los niveles séricos de Aβ1- 42, T-tau y P-Tau-181 en la práctica clínica. Además, el valor de la evaluación combinada de estos tres biomarcadores es mayor que la evaluación de estos factores individualmente.
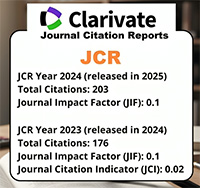
Descargas
Citas
Gustavsson A, Norton N, Fast T, Frölich L, Georges J, Holzapfel D, et al. Global estimates on the number of persons across the Alzheimer’s disease continuum. Alzheimers Dement. 2023;19(2):658-670. https://doi.org/10.1002/alz.12694.
2023 Alzheimer’s disease facts and figures. Alzheimers Dement. 2023;19(4):1598- 1695. https://doi.org/10.1002/alz.13016.
Jucker M, Walker LC. Alzheimer’s disease: From immunotherapy to immunoprevention. Cell. 2023;186(20):4260-4270. https://doi.org/10.1016/j.cell.2023.08.021.
Reuben DB, Kremen S, Maust DT. Dementia Prevention and Treatment: A Narrative Review. JAMA Intern Med. 2024;184(5):563-572. https://doi.org/10.1001/jamainternmed.2023.8522.
Rostagno AA. Pathogenesis of Alzheimer’s Disease. Int J Mol Sci. 2022;24(1):107. https://doi.org/10.3390/ijms24010107.
Ashrafizadeh M. Cell Death Mechanisms in Human Cancers: Molecular Pathways, Therapy Resistance and Therapeutic Perspective. JCBT. 2024;1(1):17-40. http://dx.doi.org/10.62382/jcbt.v1i1.13
Majidazar R, Rezazadeh-Gavgani E, Sadigh-Eteghad S, Naseri A. Pharmacotherapy of Alzheimer’s disease: an overview of systematic reviews. Eur J Clin Pharmacol. 2022;78(10):1567-1587. https://doi. org/10.1007/s00228-022-03363-6.
Jun R. Advances in Combination Therapy for Gastric Cancer: Integrating Targeted Agents and Immunotherapy. ACPT. 2024;1(1):1-15. https://doi.org/10.63623/9k14tf70
Söderberg L, Johannesson M, Nygren P, Laudon H, Eriksson F, Osswald G, et al. Lecanemab, Aducanumab, and Gantenerumab - Binding Profiles to Different Forms of Amyloid-Beta Might Explain Efficacy and Side Effects in Clinical Trials for Alzheimer’s Disease. Neurotherapeutics. 2023;20(1):195-206. https://doi.org/10.1007/s13311-022-01308-6.
Zhang J, Zhang Y, Wang J, Xia Y, Zhang J, Chen L. Recent advances in Alzheimer’s disease: Mechanisms, clinical trials and new drug development strategies. Sig Transduct Target Ther. 2024;9(1):211. https://doi.org/10.1038/s41392-024-01911-3.
Jin J, Xu Z, Zhang L, Zhang C, Zhao X, Mao Y, et al. Gut-derived β-amyloid: Likely a centerpiece of the gut-brain axis contributing to Alzheimer’s pathogenesis. Gut microbes. 2023;15(1):2167172. https://doi.org/10.1080/19490976.2023.2167172.
Hur JY. γ-Secretase in Alzheimer’s disease. Exp Mol Med. 2022;54(4):433-446. https://doi.org/10.1038/s12276-022-00754-8.
Chatterjee P, Pedrini S, Doecke JD, Thota R, Villemagne VL, Doré V, et al. Plasma Aβ42/40 ratio, p-tau181, GFAP, and NfL across the Alzheimer’s disease continuum: A cross-sectional and longitudinal study in the AIBL cohort. Alzheimers Dement. 2023;19(4):1117-1134. https://doi.org/10.1002/alz.12724.
Zeng XX, Zeng JB. Systems Medicine as a Strategy to Deal with Alzheimer’s Disease. J Alzheimers Dis. 2023;96(4):1411-1426. https://doi.org/10.3233/JAD-230739.
Perneczky R, Dom G, Chan A, Falkai P, Bassetti C. Anti-amyloid antibody treatments for Alzheimer’s disease. Eur J Neurol. 2024;31(2):e16049. https://doi.org/10.1111/ene.16049.
Young-Pearse TL, Lee H, Hsieh YC, Chou V, Selkoe DJ. Moving beyond amyloid and tau to capture the biological heterogeneity of Alzheimer’s disease. Trends Neurosci. 2023;46(6):426-444. https://doi.org/10.1016/j.tins.2023.03.005.
Ossenkoppele R, van der Kant R, Hansson O. Tau biomarkers in Alzheimer’s disease: towards implementation in clinical practice and trials. Lancet Neurol. 2022;21(8):726-734. https://doi.org/10.1016/S1474-4422(22)00168-5.
Brickman AM, Manly JJ, Honig LS, Sanchez D, Reyes-Dumeyer D, Lantigua RA, et al. Plasma p-tau181, p-tau217, and other blood-based Alzheimer’s disease biomarkers in a multi-ethnic, community study. Alzheimers Dement. 2021;17(8):1353-1364. https://doi.org/10.1002/alz.12301.
Dubois B, von Arnim CAF, Burnie N, Bozeat S, Cummings J. Biomarkers in Alzheimer’s disease: role in early and differential diagnosis and recognition of atypical variants. Alzheimers Res Ther. 2023;15(1):175. https://doi.org/10.1186/s13195-023-01314-6.
Brooker D, La Fontaine J, Evans S, Bray J, Saad K. Public health guidance to facilitate timely diagnosis of dementia: ALzheimer’s COoperative Valuation in Europe recommendations. Int J Geriatr Psychiatry. 2014;29(7):682-693. https://doi.org/10.1002/gps.4066.
Engedal K, Benth J, Gjøra L, Skjellegrind HK, Nåvik M, Selbæk G. Normative Scores on the Norwegian Version of the Mini-Mental State Examination. J Alzheimers Dis. 2023;92(3):831-842. https://doi.org/10.3233/JAD-221068.
Lima Pereira V, Freitas S, Simões MR, Gerardo B. Montreal Cognitive Assessment (MoCA): A validation study among prisoners. Crim Behav Ment Health. 2023;33(5):330-341. https://doi.org/10.1002/cbm.2306.
Monteiro C, Toth B, Brunstein F, Bobbala A, Datta S, Ceniceros R, et al. Randomized Phase II Study of the Safety and Efficacy of Semorinemab in Participants with Mild-to-Moderate Alzheimer Disease: Lauriet. Neurology. 2023;101(14):e1391-e1401. https://doi.org/10.1212/WNL.0000000000207663.
Lacorte E, Ancidoni A, Zaccaria V, Remoli G, Tariciotti L, Bellomo G, et al. Safety and Efficacy of Monoclonal Antibodies for Alzheimer’s Disease: A Systematic Review and Meta-Analysis of Published and Unpublished Clinical Trials. J Alzheimers Dis. 2022;87(1):101-129. https://doi.org/10.3233/JAD-220046.
Zhang YT, Chen Y, Shang KX, Yu H, Li XF, Yu H. Effect of Volatile Anesthesia Versus Intravenous Anesthesia on Postoperative Pulmonary Complications in Patients Undergoing Minimally Invasive Esophagectomy: A Randomized Clinical Trial. Anesth Analg. 2024;139(3):571-580. https://doi.org/10.1213/ANE.0000000000006814.
Zhu M, Xiao B, Xue T, Qin S, Ding J, Wu Y, et al. Cdc42GAP deficiency contributes to the Alzheimer’s disease phenotype. Brain. 2023;146(10):4350-4365. https://doi.org/10.1093/brain/awad184.
Kashif M, Sivaprakasam P, Vijendra P, Waseem M, Pandurangan AK. A Recent Update on Pathophysiology and Therapeutic Interventions of Alzheimer’s Disease. Curr Pharm Des. 2023;29(43):3428-3441. https://doi.org/10.2174/0113816128264355231121064704.
Giacomucci G, Mazzeo S, Crucitti C, Ingannato A, Bagnoli S, Padiglioni S, et al. Plasma p-tau181 as a promising non-invasive biomarker of Alzheimer’s Disease pathology in Subjective Cognitive Decline and Mild Cognitive Impairment. J Neurol Sci. 2023;453:120805. https://doi.org/10.1016/j.jns.2023.120805.
Yang W, Guan F, Yang L, Shou G, Zhu F, Xu Y, et al. Highly sensitive blood-based biomarkers detection of beta-amyloid and phosphorylated-tau181 for Alzheimer’s disease. Front Neurol. 2024;15:1445479. https://doi.org/10.3389/fneur.2024.1445479.
Guo J, Wang Z, Liu R, Huang Y, Zhang N, Zhang R. Memantine, Donepezil, or Combination Therapy-What is the best therapy for Alzheimer’s Disease? A Network Meta-Analysis. Brain Behav. 2020;10(11):e01831. https://doi.org/10.1002/brb3.1831.
Buck A, Rezaei K, Quazi A, Goldmeier G, Silverglate B, Grossberg GT. The donepezil transdermal system for the treatment of patients with mild, moderate, or severe Alzheimer’s disease: a critical review. Expert Rev Neurother. 2024;24(6):607-614. https://doi.org/10.1080/14737175.2024.2355981.
Zohny SM, Habib MZ, Mohamad MI, Elayat WM, Elhossiny RM, El-Salam MFA, et al. Memantine/Aripiprazole Combination Alleviates Cognitive Dysfunction in Valproic Acid Rat Model of Autism: Hippocampal CREB/BDNF Signaling and Glutamate Homeostasis. Neurotherapeutics. 2023;20(2):464-483. https://doi.org/10.1007/s13311-023-01360-w.
Savarimuthu A, Ponniah RJ. Cognition and Cognitive Reserve. Integr Psychol Behav Sci. 2024;58(2):483-501. https://doi.org/10.1007/s12124-024-09821-3.
Umarova RM, Schumacher LV, Schmidt CSM, Martin M, Egger K, Urbach H, et al. Interaction between cognitive reserve and age moderates effect of lesion load on stroke outcome. Sci Rep. 2021;11(1):4478. https://doi.org/10.1038/s41598-021-83927-1.
Hassan M, Fang S, Malik AA, Lak TA, Rizwan M. Impact of perceived social support and psychological capital on university students’ academic success: testing the role of academic adjustment as a moderator. BMC Psychol. 2023;11(1):340. https://doi.org/10.1186/s40359-023-01385-y.
Rosselli M, Uribe IV, Ahne E, Shihadeh Culture, Ethnicity, and Level of Education in Alzheimer’s Disease. Neurotherapeutics. 2022;19(1):26-54. https://doi.org/10.1007/s13311-022-01193-z.
Iso-Markku P, Kujala UM, Knittle K, Polet J, Vuoksimaa E, Waller K. Physical activity as a protective factor for dementia and Al- zheimer’s disease: systematic review, meta-analysis and quality assessment of cohort and case-control studies. Br J Sports Med. 2022;56(12):701-709. https://doi.org/10.1136/bjsports-2021-104981.
López-Ortiz S, Lista S, Valenzuela PL, Pinto-Fraga J, Carmona R, Caraci F, et al. Effects of physical activity and exercise interventions on Alzheimer’s disease: an umbrella review of existing meta-analyses. J Neurol. 2023;270(2):711-725. https://doi.org/10.1007/s00415-022-11454-8.
Fong Yan A, Nicholson LL, Ward RE, Hiller CE, Dovey K, Parker HM, et al. The Effectiveness of Dance Interventions on Psychological and Cognitive Health Outcomes Compared with Other Forms of Physical Activity: A Systematic Review with Meta-analysis. Sports Med. 2024;54(5):1179-1205. https://doi.org/10.1007/s40279-023-01990-2.
The 2023 nonhormone therapy position statement of The North American Menopause Society. Menopause. 2023;30(6):573-590. https://doi.org/10.1097/GME.0000000000002200.
Li X, Jin Y, Ding X, Zhu T, Wei C, Yao Long-term exercise training inhibits inflammation by suppressing hippocampal NLRP3 in APP/PS1 mice. Sports Med Health Sci. 2023;5(4):329-335. https://doi.org/10.1016/j.smhs.2023.09.009.
da Rosa MM, de Aguiar Ferreira M, de Oliveira Lima CA, Santos Mendonça AC, Silva YM, Sharjeel M, et al. Alzheimer’s disease: Is there a role for galectins? Eur J Pharmacol. 2021;909:174437. https://doi.org/10.1016/j.ejphar.2021.174437.
Wu W, Ji Y, Wang Z, Wu X, Li J, Gu F, et al. The FDA-approved anti-amyloid-β monoclonal antibodies for the treatment of Alzheimer’s disease: a systematic review and meta-analysis of randomized controlled trials. Eur J Med Res. 2023;28(1):544. https://doi.org/10.1186/s40001-023-01512-w.
Xiao L, Yang X, Sharma VK, Abebe D, Loh YP. Hippocampal delivery of neurotrophic factor-α1/carboxypeptidase E gene prevents neurodegeneration, amyloidosis, memory loss in Alzheimer’s Disease male mice. Mol Psychiatry. 2023;28(8):3332- 3342. https://doi.org/10.1038/s41380-023-02135-7.
Scheltens P, De Strooper B, Kivipelto M, Holstege H, Chételat G, Teunissen CE, et al. Alzheimer’s disease. Lancet. 2021;397(10284):1577-1590. https://doi.org/10.1016/S0140-6736(20)32205-4.
Cai H, Pang Y, Fu X, Ren Z, Jia L. Plasma biomarkers predict Alzheimer’s disease before clinical onset in Chinese cohorts. Nat Commun. 2023;14(1):6747. https://doi.org/10.1038/s41467-023-42596-6.