Evaluación del efecto terapéutico de una pomada a base de propóleos argelinos sobre heridas por quemaduras en conejos
Resumen
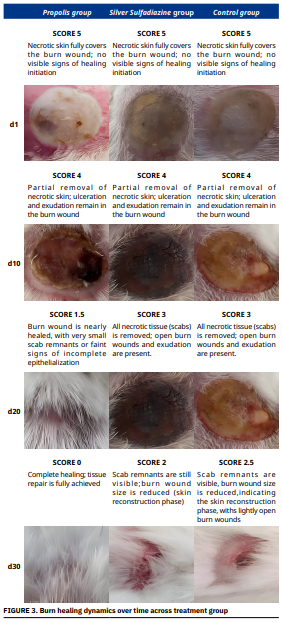
Este estudio evalúa la eficacia terapéutica del propóleo argelino en el tratamiento de quemaduras superficiales de segundo grado, combinando ensayos antibacterianos in vitro y experimentos de cicatrización in vivo. Las pruebas in vitro revelaron que, aunque la sulfadiazina de plata mostró una actividad antibacteriana superior contra Staphylococcus aureus, la muestra de propóleos P2 presentó un efecto inhibidor significativo (19,35 ± 2,29 mm). Esta variabilidad en la acción antimicrobiana entre las muestras de propóleos podría atribuirse a diferencias en la composición química, reflejo de la diversidad botánica de su origen. En el modelo in vivo, la aplicación tópica de propóleos demostró resultados de cicatrización notablemente mejores en comparación con la sulfadiazina de plata y el grupo control no tratado. Todos los grupos comenzaron con una severidad de quemadura idéntica el día (d) 1 (puntuación de cicatrización = 5). A partir del d 20, el grupo tratado con propóleos mostró una regeneración tisular significativamente más rápida, con cierre completo de la herida (puntuación = 0) logrado al d En cambio, el grupo tratado con sulfadiazina alcanzó solo un 84,5% de contracción al d 33, y el grupo control mostró una cicatrización incompleta (hasta un 88,3%). Las puntuaciones medias acumuladas de cicatrización respaldaron aún más el mejor desempeño del propóleos (2,79 ± 1,44), en comparación con la sulfadiazina (3,70 ± 1,16) y el control (3,74 ± 0,68). Además, se observó un crecimiento precoz del pelo en los animales tratados con propóleos, lo que sugiere una mejor regeneración cutáne Es importante destacar que no se observó alteración de la regulación de la temperatura corporal en ninguno de los grupos, lo que indica la seguridad del uso del propóleos. En conclusión, el propóleos argelino muestra tanto una actividad antibacteriana moderada como excelentes propiedades cicatrizantes, favoreciendo una regeneración cutánea rápida y completa. Su origen natural, facilidad de aplicación y capacidad regenerativa lo posicionan como una alternativa prometedora para el tratamiento de quemaduras superficiales. Se recomiendan estudios adicionales para investigar los mecanismos implicados y optimizar su formulación para uso clínico.
Descargas
Citas
Shpichka A, Butnaru D, Bezrukov EA, Sukhanov RB, Atala A, Burdukovskii V, Zhang Y, Timashev P. Skin tissue regeneration for burn injury. Stem Cell Res. Ther. [Internet]. 2019; 10(1):94. doi: https://doi.org/gkzftt DOI: https://doi.org/10.1186/s13287-019-1203-3
Li HL, Deng YT, Zhang ZR, Fu QR, Zheng YH, Cao XM, Nie J, Fu LW, Chen LP, Xiong YX, Shen DY, Chen QX. Evaluation of effectiveness in a novel wound healing ointment—crocodile oil burn ointment. Afr. J. Tradit. Complement. Altern. Med. [Internet]. 2016; 14(1):62–72. doi: https://doi.org/qgv2 DOI: https://doi.org/10.21010/ajtcam.v14i1.8
El Baassiri MG, Dosh L, Haidar H, Gerges A, Baassiri S, Leone A, Rappa F, Jurjus A. Nerve growth factor and burn wound healing: Update of molecular interactions with skin cells. Burns [Internet]. 2023; 49(5):989–1002. doi: https://doi.org/qgv3 DOI: https://doi.org/10.1016/j.burns.2022.11.001
Yang J, Pi A, Yan L, Li J, Nan S, Zhang J, Hao Y. Research progress on therapeutic effect and mechanism of propolis on wound healing. Evid. Based Complement. Alternat. Med. [Internet]. 2022; 2022:5798941. doi: https://doi.org/pqw5 DOI: https://doi.org/10.1155/2022/5798941
Lu M, Zhao J, Wang X, Zhang J, Shan F, Jiang D. Research advances in prevention and treatment of burn wound deepening in early stage. Front. Surg. [Internet]. 2022; 9:1015411. doi: https://doi.org/qgv4 DOI: https://doi.org/10.3389/fsurg.2022.1015411
Afata TN, Dekebo A. Chemical composition and antimicrobial effect of western Ethiopian propolis. Chem. Biodivers. [Internet]. 2023; 20(2):e202200922. doi: https://doi.org/qgv5 DOI: https://doi.org/10.1002/cbdv.202200922
Dekebo A, Geba C, Bisrat D, Jeong JB, Jung C. Wound healing, anti–inflammatory and antioxidant activities, and chemical composition of Korean propolis from different sources. Int. J. Mol. Sci. [Internet]. 2024; 25(21):11352. doi: https://doi.org/qgv6 DOI: https://doi.org/10.3390/ijms252111352
Soltani E, Mokhnache K, Charef N. Polyphenol contents and antioxidant activity of ethanolic and aqueous Algerian propolis extracts (region of Serdj el Ghoul). J. Drug. Deliv. Ther. [Internet]. 2020; 10(1):1–4. doi: https://doi.org/qgv8 DOI: https://doi.org/10.22270/jddt.v10i1.3797
Zhang A, Chen X, Hussain SA, Alrubie TM, Maddu N, Zhang Q. Anesthetic wound dressing loaded with propolis and bupivacaine for managing post–operative pain and wound healing. J. Bioact. Compat. Polym. [Internet]. 2025; 40(3):229-247. doi: https://doi.org/qgv9 DOI: https://doi.org/10.1177/08839115251329379
Cornara L, Biagi M, Xiao J, Burlando B. Therapeutic properties of bioactive compounds from different honey bee products. Front. Pharmacol [Internet]. 2017; 8:412. doi: https://doi.org/mjfw DOI: https://doi.org/10.3389/fphar.2017.00412
Oryan A, Alemzadeh E, Moshiri A. Potentialrole of propolis in wound healing: Biological properties and therapeutic activities. Biomed. Pharmacother. [Internet]. 2018; 98:469–483. doi: https://doi.org/gc57z5 DOI: https://doi.org/10.1016/j.biopha.2017.12.069
Boudra A, Benbelkacem I, Aissa MA. Antibacterial activity of different ethanolic extracts of Algerian propolis against Staphylococcus aureus. Bionature [Internet]. 2019 [cited Jun 22, 2025]; 40(1):4–8. Available in: https://goo.su/3zVHC
Boudra A, Merati R, Abdelkader B, Yezli W, Helali H, Henni I. Therapeutic properties of Algerian propolis in skin wound healing with significant tissue loss. Rev. Cient. FCV–LUZ. [Internet]. 2025; 35(2):e35658. doi: https://doi.org/qgwc DOI: https://doi.org/10.52973/rcfcv-e35658
Boudra A, Merati R, Berrani A, Yezli W, Hocine L, Benbeguara M, Zineddine E. Role of Algerian propolis on hemato–biochemical parameters and bone consolidation mechanisms in rabbits receiving autoclaved diaphyseal allografts. Rev. Cient. FCV–LUZ [Internet]. 2024; 35(3):e35677. doi: https://doi.org/qgwd DOI: https://doi.org/10.52973/rcfcv-e35677
Balouiri M, Sadiki M, Ibnsouda SK. Methods for in vitro evaluating antimicrobial activity: A review. J. Pharm. Anal. [Internet]. 2016; 6(2):71–79. doi: https://doi.org/gfwdq2 DOI: https://doi.org/10.1016/j.jpha.2015.11.005
Couquet Y, Desmoulière A, Rigal ML. The Antibacterial and cicatrising properties of honey. Actual. Pharm. [Internet]. 2013; 52(531):22–25. doi: https://doi.org/qgwf DOI: https://doi.org/10.1016/j.actpha.2013.10.005
Boudra A, Benbelkacem I, Merati R, Achour H, Daouadji ID. Comparison between three fixed anaesthesia protocols in rabbits. J. Prev. Vet. Med. [Internet]. 2020; 44(3):99–103. doi: https://doi.org/pqw3 DOI: https://doi.org/10.13041/jpvm.2020.44.3.99
Sene M, Barboza FS, Top B, Ndiaye M, Sarr A, Fall AD, Sy GY. Wound healing activity of the aqueous leaf extract of Elaeis guineensis Jacq. (Arecaceae). Int. J. Biol. Chem. Sci. [Internet]. 2020; 14(3):674–684. doi: https://doi.org/pqwz DOI: https://doi.org/10.4314/ijbcs.v14i3.3
Adhya A, Bain J, Ray O, Hazra A, Adhikari S, Dutta G, Ray S, Majumdar BK. Healing of burn wounds by topical treatment: A randomized controlled comparison between silver sulfadiazine and nano–crystalline silver. J. Basic. Clin. Pharm. [Internet]. 2015 [cited Jun 22, 2025]; 6(1):29–34. Available in: https://goo.su/qM3G1 DOI: https://doi.org/10.4103/0976-0105.145776
Wendelken ME, Berg WT, Lichtenstein P, Markowitz L, Comfort C, Alvarez OM. Wounds measured from digital photographs using photodigital planimetry software: Validation and rater reliability. Wounds [Internet]. 2011 [cited Jun 22, 2025]; 23(9):267–275. PMID: 25879267. Available in: https://goo.su/zsGJv
Subalakshmi M, Saranya A, Maheswari MU, Jarina A, Kaviman S, Murali R. An overview of the current ethodologies used for the evaluation of drugs having wound healing activity. Int. J. Exp. Pharmacol. [Internet]. 2014 [cited Jun 20, 2025]; 4(2):127–131. Available in: https://goo.su/Gh9O
Daraghmeh J, Imtara H. In vitro evaluation of Palestinian propolis as a natural product with antioxidant properties and antimicrobial activity against multidrug–resistant clinical isolates. J. Food Qual. [Internet]. 2020; 2020:8861395. doi: https://doi.org/qg3r DOI: https://doi.org/10.1155/2020/8861395
Sarkez NH. Antimicrobial properties of Libyan propolis against Staphylococcus aureus. Libyan J. Med. Res. [Internet]. 2014; 8(1):50–55. doi: https://doi.org/qg3s DOI: https://doi.org/10.54361/ljmr.v8i1.09
Dégi J, Herman V, Igna V, Dégi DM, Hulea A, Muselin F, Cristina RT. Antibacterial activity of Romanian propolis against Staphylococcus aureus isolated from dogs with superficial pyoderma: In vitro test. Vet. Sci. [Internet]. 2022; 9(6):299. doi: https://doi.org/qg3t DOI: https://doi.org/10.3390/vetsci9060299
El–Guendouz S, Lyoussi B, Miguel MG. Insight on propolis from Mediterranean countries: Chemical composition, biological activities and application fields. Chem. Biodivers. [Internet]. 2019; 16(7):e1900094. doi: https://doi.org/qg3v DOI: https://doi.org/10.1002/cbdv.201900094
Will C. Hypothermia, hyperthermia and fever syndrome in pet rabbits. Nouv. Prat. Vet. Canine & Feline. [Internet]. 2024; 21(87):14–21. doi: https://doi.org/qg3w DOI: https://doi.org/10.1051/npvcafe/2024027
Salibian AA, Del Rosario AT, De Almeida Moura Severo L, Nguyen L, Banyard DA, Toranto JD, Evans GRD, Widgerow AD. Current concepts on burn wound conversion—A review of recent advances in understanding the secondary progressions of burns. Burns [Internet]. 2016; 42(5):1025–1035. doi: https://doi.org/f8z3sx DOI: https://doi.org/10.1016/j.burns.2015.11.007
Jastrzębska–Stojko Ż, Stojko R, Rzepecka–Stojko A, Kabała– Dzik A, Stojko J. Biologicalactivity of propolis–honeybalm in the treatment of experimentally–evoked burn wounds. Molecules [Internet]. 2013; 18(11):14397–14313. doi: https://doi.org/f5ncw7 DOI: https://doi.org/10.3390/molecules181114397
Gregory SR, Piccolo N, Piccolo MT, Piccolo MS, Heggers JP. Comparison of propolis skin cream to silver sulfadiazine: A naturopathic alternative to antibiotics in treatment of minor burns. J. Altern. Complement. Med. [Internet]. 2002; 8(1):77–83. doi: https://doi.org/c445xz DOI: https://doi.org/10.1089/107555302753507203
Kalil MA, Santos LM, Barral TD, Rodrigues DM, Pereira NP, Sá MDCA, Umsza–Guez MA, Machado BAS, Meyer R, Portela RW. Brazilian green propolis as a therapeutic agent for the post– surgical treatment of caseous lymphadenitis in sheep. Front. Vet. Sci. [Internet]. 2019; 6:399. doi: https://doi.org/gn7268 DOI: https://doi.org/10.3389/fvets.2019.00399
Abu–Seida AM. Effect of propolis on experimental cutaneous wound healing in dogs. Vet. Med. Int. [Internet]. 2015; 2015:672643. doi: https://doi.org/gcfgcr DOI: https://doi.org/10.1155/2015/672643
El–Kersh DM, Abou El–Ezz RF, Ramadan E, El–Kased RF. In vitro and in vivo burn healing study of standardized propolis: Unveiling its antibacterial, antioxidant and anti–inflammatory actions in relation to its phytochemical profiling. PLoS One [Internet]. 2025;20(2):e0319204. doi: https://doi.org/qg3x DOI: https://doi.org/10.1371/journal.pone.0319204
Manginstar CO, Tallei TE, Niode NJ, Salaki CL, Hessel SS. Therapeutic potential of propolis in alleviating inflammatory response and promoting wound healing in skin burn. Phytother. Res. [Internet]. 2024; 38(2):856–879. doi: https://doi.org/qg34 DOI: https://doi.org/10.1002/ptr.8092
Akpınar A, Özdemir H. Effect of propolis on wound healing: A clinical and histomorphometric study in rats. J. Biotechnol. Strateg. Health Res. [Internet]. 2023; 7(2):81–88. doi: https://doi.org/qg37 DOI: https://doi.org/10.34084/bshr.1289441
Carvalho MT, Araújo–Filho HG, Barreto AS, Quintans–Júnior LJ, Quintans JSS, Barreto RSS. Wound healing properties of flavonoids: A systematic review highlighting the mechanisms of action. Phytomedicine [Internet]. 2021; 90:153636. doi: https://doi.org/qg35 DOI: https://doi.org/10.1016/j.phymed.2021.153636
Olczyk P, Wisowski G, Komosinska–Vassev K, Stojko J, Klimek K, Olczyk M, Kozma EM. Propolis modifies collagen types I and III accumulation in the matrix of burnt tissue. Evid. Based Complement. Alternat. Med. [Internet]. 2013; 2013:423809. doi: https://doi.org/gb6nb7 DOI: https://doi.org/10.1155/2013/423809
Salrian AA, Behzadi A, Oloumi MM, Farajli Abbasi M, Delshad S, Moghadaszadeh M. Amplification of wound healing by propolis and honey ointment in healthy and diabetic rat models: Histopathological and morphometric findings. Arch. Razi Inst. [Internet]. 2022; 77(5):1673–1681. doi: https://doi.org/qg39